Below is the picture of a virus replication cycle.
From this picture, we can see that the virus undergoes 6 steps, mainly:
- - Attachment
- - Penetration
- - Uncoating
- - Replication & Expression
- - Maturation
- - And finally, the release of the Virus.
We'll cover in details, the different stages of virus replication at a later part.
This is what most of the virus will generally go through. However, there are also different types of the replication cycle.
- 1. Lytic Cycle
- 2. Lysogenic Cycle

(Image adapted from: http://www.prism.gatech.edu/~gh19/b1510/8lytic.jpg)
1. Firstly, attachment must occur before the virus goes into lytic or lysogenic cycle.
2. The phage DNA circularizes and enters lytic cycle or lysogenic cycle.
In the Lytic cycle:
3(i). New phage DNA and proteins are synthesized and assembeled into virions.
4(i).Cell lyses, releasing phage virions.
5(i). The cycle goes on again.
In the Lysogenic cycle:
3(ii). Phage DNA integrates within the bacterial chromosome by recombination, becoming a prophage.
4(ii). Lysogenic bacteria reproduces normally (undergoes many cell devisions).
5(ii). Occassionally, the prophage may seperate from the cell by another recombinant event, initiating a lytic cycle.
Now, we'll look into the Attachment stage.
1. Viral Attachment or Adsorption to the Host Cell
Adsorption (def: The attachment of one substance to the surface of another, eg, a virus attaching to a receptor on the surface of a susceptible host cell.) involves the binding of attachment sites on the viral surface with receptor sites on the host cell cytoplasmic membrane.
For a virus to infect a host cell, the cell must have specific receptors (ie, protein, glycoprotein or glycolipid) for the virus on its surface and also be capable of supporting viral replication. These host cell receptors are normal surface molecules involved in routine cellular function, but since a portion of a molecule on the viral surface resembles the chemical shape of the body's molecule that would normally bind to the receptor, the virus is able to attach to the host cell's surface.
An example is the Hepatitis B virus. The hepatitis B virus (HBV) adsorbs to IgA receptors on human cells. These receptors normally bind the antibody isotype IgA for transport across cells.
(Image adapted from: http://student.ccbcmd.edu/courses/bio141/lecguide/unit3/viruses/ev_adsorb.html)
The cell receptor site are specific. Virus binds to specific receptors on the host cell.
If the receptor on the host cell does not cater to the virus, then attachment will not happen.
(Image adapted from: http://www.goalfinder.com/product.asp?productid=151)
These are some of the receptors of certain host cells.
2. Penetration
Penetration into eukaryotic cells occurs in 3 ways:
- Endocytosis
- - Receptor-Mediated (enveloped virus)
- - Clathrin (naked virus)
- Fusion (enveloped virus)
(i) Endocytosis - Receptor-Mediated
(Image adapted from: http://academic.brooklyn.cuny.edu/biology/bio4fv/page/rectpr.htm)
The virus first binds to the receptor, then endocytosis happens.
(ii) Endocytosis - Clathrin
1. Attachment sites on the virus bind to corresponding receptors on the host cell membrane.
2. The virus begins to enter the host cell by endocytosis
3. The entire virus is placed in an endocytic vesicle.
4. The entire virus is placed in an endocytic vesicle.
(iii) Fusion
1. Attachment sites on the virus bind to corresponding receptors on the host cell membrane.
2. The viral envelope fuses with host cell's cytoplasmic membrane and nucleocapsid enters the host cell.
3. The viral envelope fuses with host cell's cytoplasmic membrane and nucleocapsid enters the host cell.











 5. MATURATION
5. MATURATION
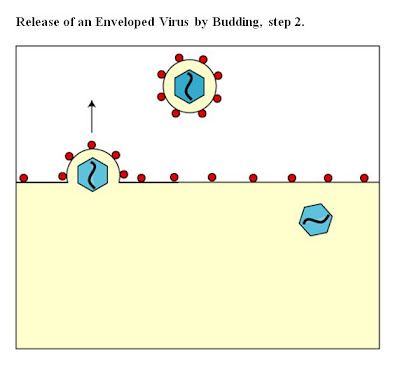
 6. RELEASE
6. RELEASE b. Enveloped viruses
b. Enveloped viruses